Spinal Muscular Atrophy: Causes and importance of early diagnosis for proactive management
A person with SMA may find it challenging to stand up, walk, control their head movements, and in some cases, even breathe and swallow
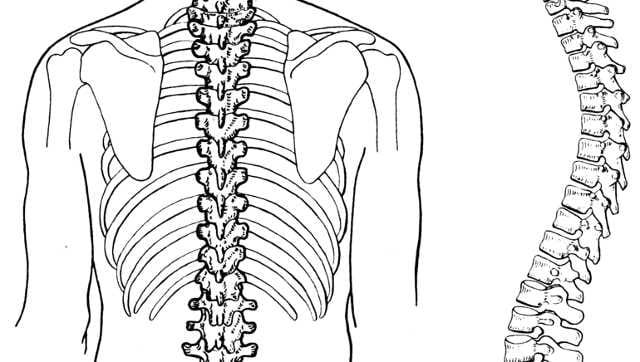
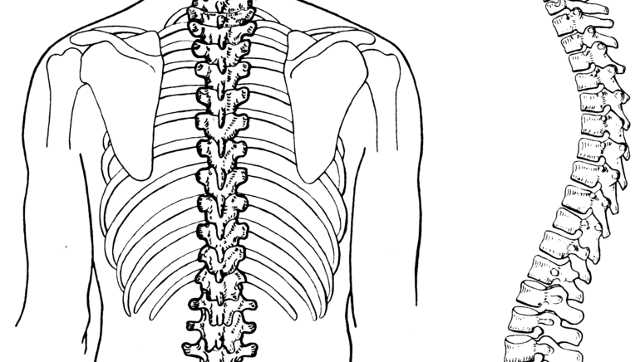
Spine. Image courtesy Pearson Scott Foresman/Wikimedia Commons
Spinal muscular atrophy (SMA) is a severe genetic condition that targets motor neurons in the central nervous system (CNS), resulting in progressive muscle atrophy, weakness, and paralysis. It is a group of genetic disorders in which a person cannot control the movement of their muscles due to a loss of nerve cells in the spinal cord and brain stem. A person with SMA may find it challenging to stand up, walk, control their head movements, and in some cases, even breathe and swallow. Some forms of SMA are present at birth, while others develop over time. Some have an impact on life expectancy.
SMA can be clinically divided into five subtypes. The most severe type is SMA type 0, appear before birth, can be fatal before or after birth within the first year of life. Type 1 SMA also called infantile-onset, is the most common type of SMA, accounting for 60% cases, which appears in infants and causes them to die or become dependent on a ventilator by the age of two. Children with SMA type 2 are sitters, while those with type 3 can walk on their own for a while before becoming wheelchair-bound. SMA type 4 develops in adults and causes later-life progressive weakness.
SMA is the most frequent cause of death in the infantile age group, occurring in one in 10,000 live births. However, the SMA carrier frequency was 1 in 38 in a recent Indian study. Children with SMA can currently receive supportive care in India that includes assisted ventilation, feeding, physiotherapy, orthotics, and spine stabilization.
What causes SMA?
SMA is caused by a very specific genetic mutation in a gene called the SMN1 gene. SMN is that protein that play a critical role in the survival of the nerve cells that control muscles. (SMN) protein keeps motor neurons healthy and functioning normally. The loss of motor neurons in the spinal cord caused by SMA patients, and insufficient levels of the SMN protein results in skeletal muscle weakness and wasting.
SMA patients gradually lose their ability to control their muscles movement and strength. The muscles closest to the torso and neck are frequently severely affected by the disease. Some SMA patients never sit, stand, or walk. Other signs of SMA include tongue fasciculation, a bell-shaped chest (caused by muscle weakness), weak cough, difficulty breathing , choking or trouble swallowing, weak sucking and labored breathing during feeding.
How is SMA diagnosed?
The diagnosis of spinal muscular atrophy depends on the type of SMA a person has and age of onset. The path to diagnosis for infants and children with more severe forms of SMA frequently starts when a parent or medical professional notices unusual muscle weakness (hypotonia). People with adult-onset SMA types, such as type 4, might begin the diagnosis process after observing minor symptoms like hand tremors.
Physical exam
A physical examination is required to identify the presence of symptoms like muscle weakness or a lack of reflexes in cases where a new-born is not screened for SMA at birth. A primary care physician or a neurologist could perform this.
Family medical history
As part of your or your child’s physical examination, a thorough review of the patient’s family history is necessary to determine whether there have ever been any instances of neuromuscular disease in the family. If the physical examination and family history raise suspicion of SMA, genetic testing will likely be the next step.
Genetic testing
Through molecular genetic testing, which requires a blood sample, SMA is identified. A single gene is examined for mutations linked to a genetic disease in molecular genetic testing.
Importance of early diagnosis
A patient with SMA must first undergo a higher level of cognitive evaluation. The clinician should assess the patient for weakness before concentrating solely on SMA. A muscle biopsy could be the next step in the evaluation to more precisely distinguish between muscle weakness and nerve weakness. Finally, the clinician would probably identify this patient’s SMA based on the results of the combined muscle biopsy and electrode diagnostics.
If a diagnosis is made early, the individual has access to the tools and the resources that medical science has developed over the last number of years to assist optimal functioning.
The standard method for diagnosing SMA is molecular genetic testing. SMA should be given early consideration in any infant with weakness or hypotonia due to the effectiveness of molecular testing and high frequency of SMA in the hypotonic infant. All other infant causes of hypotonic weakness are included in the differential diagnosis of severe forms of SMA.
SMA is inherited in an autosomal recessive manner. Each pregnancy of a couple who have had a child with SMA has an approximately 25 per cent chance of producing an affected child. Carrier testing for at-risk relatives and prenatal testing for pregnancies at increased risk are possible if the diagnosis of SMA has been confirmed by molecular genetic testing in an affected family member.
Currently, there are several SMA treatments that have received FDA approval including Risdiplam (Evrysdi), Onasemnogene abeparvovec-xioi (Zolgensma) and Nusinersen (Spinraza). These targeted treatments may prevent the development or slow the progression of some features of SMA.
The severity of the disease varies depending on the type of SMA, with more severe subtypes needing more aggressive treatment. Proactive care and treatment decision-making by the multidisciplinary team and family are of paramount importance.
The author is MBBS, DCH, MRCPCH, Fellowship Pediatric Genetics, Consultant Clinical Geneticist, Salem Genetics Centre. Views are personal.
Read all the Latest News, Trending News, Cricket News, Bollywood News,
India News and Entertainment News here. Follow us on Facebook, Twitter and Instagram.
For all the latest health News Click Here